Table of Contents
What is Gastritis?
Gastritis is a prevalent pathology. About 50% of the world’s population suffers from it periodically. The stomach has cells responsible for producing gastric juices, damaging the tissues they come into contact with.
Usually, this does not happen because there is a mucous layer inside the stomach that neutralizes them: the gastric mucosa.
However, when this protective barrier damaged for various reasons that we will discuss in detail, the protection of the stomach from gastric juices reduce, and an inflammatory process is known as gastritis is triggered.
How Many Types of Gastritis are There?
Based on the location of the inflammation, gastritis can classify as:
Type A or antral gastritis: inflammation localizes in the final, and therefore lower part of the stomach called the antrum.
Type B or fundus gastritis: inflammation localizes in the uppermost portion of the stomach called the fundus.
A separate discussion deserves the so-called nervous gastritis, a psychosomatic pathology with symptoms very similar to normal.
Characteristics of Gastritis

Let’s see in detail the characteristics of each of these forms.
1. Acute Gastritis
- This form is characterized by a sudden and rapid onset of symptoms, with a usually short duration.
- Acute gastritis usually manifests itself with intense pain, unlike chronic gastritis, which, coming more gradually, is generally characterized by duller pain.
- In most cases, this form is caused by taking nonsteroidal anti-inflammatory drugs (NSAIDs).
- Other causes can be alcohol abuse or poor nutrition.
2. Chronic Gastritis
- In the chronic form, the inflammatory state of the gastric mucosa does not heal spontaneously but tends to persist over time. The evolution of the disease can lead to the gradual destruction of the stomach glands.
- Chronic gastritis is divided into several etiological types, depending on its cause:
- Type gastritis (about 5% of cases), caused by an autoimmune reaction. The immune system destroys some cells of the gastric mucosa, which mistakenly see as foreign;
- Type B gastritis (about 60% of cases), caused by Helicobacter Pylori (HP) infection ;
- Type C gastritis (about 30% of cases) cause by chemicals harmful to the gastric mucosa, such as alcohol, nicotine, NSAIDs (Non-Steroidal Anti-inflammatory Drugs) bile reflux.
- There may also be rare forms, such as Crohn’s disease, eosinophilic gastritis, lymphocytic gastritis, etc.
3. Nervous Gastritis
- The condition commonly and loosely referred to as gastritis Nervosa deserves mention in its own right.
- The symptoms, in this case, manifest themselves as a result of various kinds of worries, or hectic working life or conditions of suffering due to painful or traumatic events.
- Symptoms are equivalent to those of other forms of it.
Causes and Risk Factors of Gastritis
- The causes of the weakening of the defensive barrier of the stomach can be many and varied. Therefore, also for the reasons, a distinction must be made between the various forms of this disorder.
- As we have seen in the previous paragraph, chronic gastritis can be autoimmune due to infection with HP or chemicals harmful to the gastric mucosa. At the same time, the nervous one is due to psychosomatic factors.
- For the acute form, the causes are primarily due to exogenous damage, such as excess alcohol, drugs (particularly NSAIDs, associated with a critical risk of ulcer and bleeding, especially if taken continuously). More rarely, the cause may be due to infections and trauma.
- The excesses of harmful substances, such as alcohol and smoking, can be avoided. Having correct behaviours in this sense is the first form of prevention of acute conditions.
- On the other hand, chronic HP infection is strongly related to the family environment and usually contracted in childhood. There is a hypothesis that HP infection is also triggered by an autoimmune reaction, leading to chronic autoimmune gastritis.
Symptoms of Gastritis
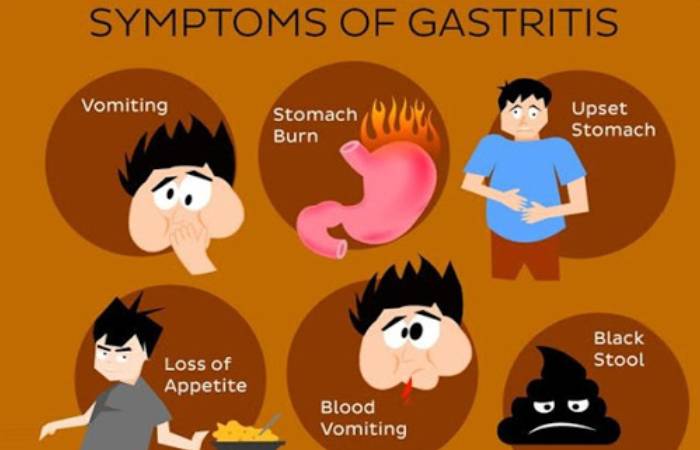
- It often remains completely asymptomatic, especially chronic. It is diagnosed occasionally, through a gastroscopy performed for other reasons or due to persistent anaemia found in laboratory tests.
- The most common symptom of chronic autoimmune gastritis is dyspepsia (a sense of heaviness and difficulty indigestion). In addition, this form can result in a particular form of pernicious anaemia, characterized by more prominent than normal red blood cells.
- Dyspepsia is due to some antibodies that affect and destroy the stomach’s parietal cells responsible for the production of hydrochloric acid and, therefore, for digestion.
- Instead, pernicious anaemia is due to the destruction by some antibodies of the intrinsic factor, a substance essential for the absorption of vitamin B12, which is necessary to produce red blood cells.
Other symptoms that may occur are:
- lack of appetite;
- nausea and vomit;
- epigastric pain (in the upper abdomen);
- heartburn;
- halitosis.
Complications of Gastritis
The main problem of acute gastritis is the risk of erosions, in some cases of an absolute gastrointestinal ulcer caused by the self-digestion of the epithelium by acid or pepsin.
Complications related to chronic gastritis are, in addition to the aforementioned pernicious anaemia and dyspepsia, the development of gastric ulcers (in 45-70% of cases due to Helicobacter Pylori infection ).
Compared to the population average, the a higher risk to develop stomach cancer or lymphoma (1 in 3,000 and 1 in 40,000, respectively).
Diagnosis of Gastritis
If you have symptoms that make you suspect, contact your doctor, who may prescribe some tests or refer you to a doctor specialising in digestive disorders ( gastroenterologist ).
Among the possible tests to be done to diagnose gastritis, there are:
Blood tests: Blood tests may aim at detecting the presence of antibodies to HP.
Stool examination: Aimed at discovering the presence of Helicobacter Pylori.
X-ray: Carried out on the stomach and small intestine, usually after taking barium, a liquid that lines the mucous membranes makes them more visible on the X-ray film.
Gastroscopy: It allows the doctor to check if abnormalities in the upper gastrointestinal tract are not detectable with an X-ray.
Warning: the diagnosis of chronic gastritis is always and only histological. This means that the patient must have had a gastroscopy with biopsies.
Treatment and Drug Therapy of Gastritis
The therapy to follow depends on the cause of gastritis:
- A lifestyle change is constructive if harmful agents cause gastritis. As already mentioned, especially acute gastritis have a good prognosis.
- Conversely, it caused by bacteria must treat with intensive antibiotic therapy due to the increased risk of malignant degeneration. The success of the treatment must ascertain.
- In the case of HP, there are various eradicating schemes and the type of therapy discuss with the patient. After alleged eradication, this must confirm by Breath Test, Breath Test, or other methods to assess the presence of HP. In some cases, gastroscopy with biopsies must repeat.
- Autoimmune gastritis is challenging to treat. Vitamin B12 can replace with injections to bypass gastrointestinal absorption failure.
- And frequent but not abundant meals recommend reducing dyspepsia. If there is a parallel HP infection, it must treat with antibiotics, and in some cases, regression of autoimmune gastritis can observe.
- In case of complications, such as an ulcer or gastric mucosal erosion, acid production can inhibit PPIs (proton pump inhibitor drugs).
- Thereby reducing symptoms and increasing the chances of recovery. If this does not help and serious complications occur, such as stomach perforation, immediate emergency intervention requires.
- Due to the possible serious complications (ulcer, carcinoma), it should always control and, if possible, treated.
- In any case, if you think you are suffering from it, we recommend that you always contact your doctor, who will recommend the most suitable therapy for your situation.
Natural Remedies to Cure Gastritis
- In addition to the tips already given above for an anti-gastritis eating style, it is also essential to take care of your general well-being.
- In this sense, and especially in cases of nervous gastritis, it is good to learn to keep stress under control.
- An excessively hectic and stressful life can increase the production of gastric acids and slow digestion, favouring its onset.
- For this reason, it is essential to find your way to relax: you can try yoga or tai chi, or with massages, all techniques that help reduce physical tension and decrease anxiety.
- Even physical activity regularly is helpful, both to release stress both to promote intestinal motility.
- There are no recommended sports or sports restrictions for sufferers, so you can choose the sport that suits you best.
- As for possible plant adjuvants, such as herbal teas or herbal infusions, they can use as an additional and not a replacement therapy. And always after appropriate consultation with your doctor.
- However, to give you a primary indication, we asked the Herbalist Alessia Onorati of La Piccola Erboristeria to suggest some treatments with herbs against it.
Conclusion
For those who suffer from it, it means heartburn, stomach acid, cramps, difficulty digesting, gastroesophageal reflux, bad breath and nausea. A series of very annoying ailments that, especially in chronic gastritis cases, can also pose a risk to general health.